2-Year-Old Female Patient from Guatemala Born with Esophageal Atresia and Tracheoesophageal Fistula (Hendren Patient Case)
- 2-year-old female patient from Guatemala born with esophageal atresia and tracheoesophageal fistula (TEF).
- She had been treated by division and closure of TEF, gastrostomy, and marsupialization of the upper esophagus into the left neck.
- She was referred to Richard H. Sweet, M.D., at Massachusetts General Hospital in October 1953. Dr. Sweet brought her stomach to her neck to restore her gastrointestinal continuity. It was my privilege to be a surgical resident on Dr. Sweet’s service at that time.
- By chance, 26 years later, she was sent to me for symptoms of severe gastritis, in her own words, “like a volcano in my chest,” and fullness after eating with respiratory distress by compression of her left lung when her stomach was full.
- Her stomach emptied very slowly on Barium examination. Pyloroplasty had not been done when she was a baby.
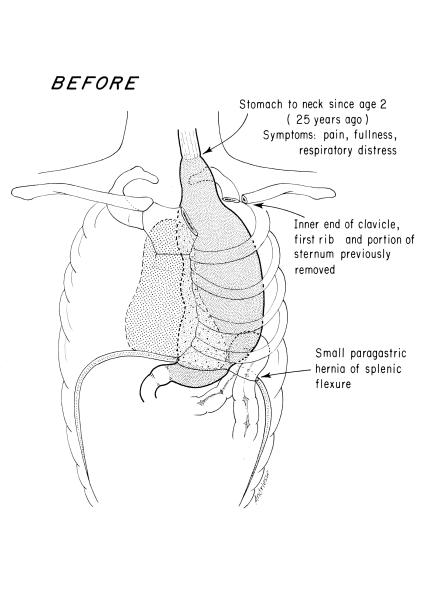
Fig. 1. Pre-Operative Anatomy. Gastric “pull-up operation” done in childhood.

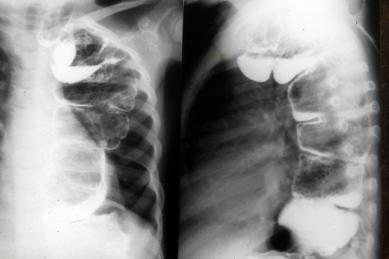
Fig. 2. Barium Filled Stomach. Upper G.I. series age 28 years, with severe symptoms secondary to stomach in the thorax.
Treatment Strategy
- In a 13-hour thoracoabdominal and left neck procedure in November 1979, the stomach was mobilized and placed back in the abdomen.
- Generous pyloroplasty was performed.
- Colon esophagus was fashioned from the transverse colon, anastamosing its hepatic flexure end-to-end with the cervical esophagus and its splenic flexure to the back wall of the stomach.
- Blood supply of the conduit was left colic and left half of the mid colic artery.
- Right gastroepiploic vessel was carefully spared, being the principal vessel perfusing the stomach.
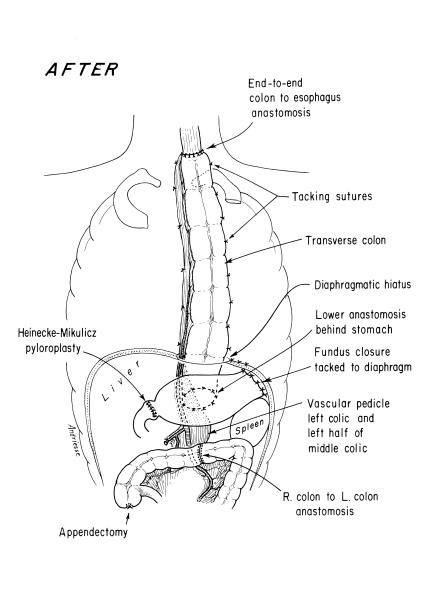
Fig. 3. Post-Operative Anatomy. Esophagoscopy immediately preceding the surgery interestingly showed no esophagitis in the segment just proximal to the gastric fundus in the upper thorax. The scope could pass easily all the way into the duodenum without encountering inflammatory changes.
Follow Up
- Patient convalesced uneventfully and returned to Guatemala, where we had the pleasure of visiting her the following year. She was asymptomatic.
- In 1984, she returned to Boston with symptoms of epigastric discomfort 2 hours after meals.
- Various medications were used, with only transient relief.
- Gastroscopy by an experienced gastroenterologist disclosed no cause for symptoms.
- Infusion of acid, saline, alkali, or her gastric juice did not cause her symptoms.
- Sucralfate was prescribed.
- Patient last seen in 1997, at age 46 years, by a second, very experienced gastroenterologist.
- Endoscopy of the colon esophagus and the stomach were unremarkable.
- No additional contact.