- 20-year-old female had esophageal atresia with tracheoesophageal fistula (TEF) successfully repaired at birth in a nearby hospital.
- At age 17 years, we saw her for a “cold nodule” of the left thyroid.
- Hemithyroidectomy was performed for what proved to be a follicular adenoma
- Barium swallow at that age showed dysmotility of the esophagus commonly seen following repair of esophageal atresia, but not gastroesophageal reflux or other abnormality.
- She now had a history of dysphagia for 3 mo when swallowing solid foods, and a weight loss of 4.5 kg (10 pounds).
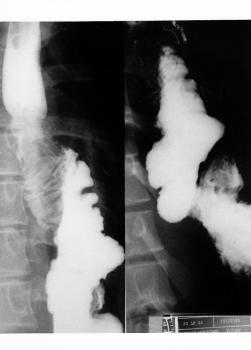
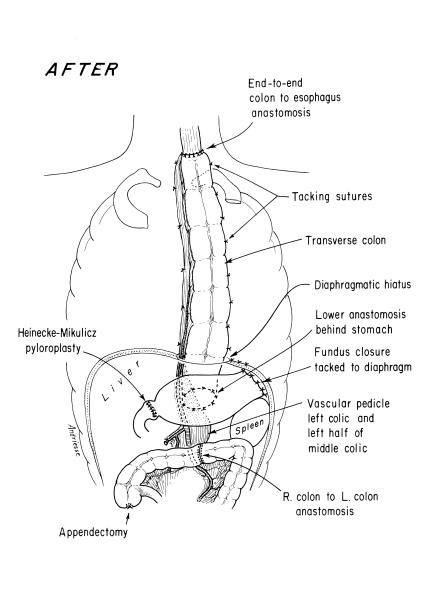
- Barium swallow showed an intraluminal mass at the esophagogastric junction.

Fig. 1. Pre-Operative Barium Swallow (Select Image for High-quality Version). This demonstrates an irregular intraluminal lesion at and above the gastroesophageal junction.

Fig. 2. Endoscopic View of Upper End of Esophagogastric Adenocarcinoma (Select Image for High-quality Version). Esophagoscopy showed an obvious carcinoma of the esophagus, a well differentiated adenocarcinoma histologically.
Treatment Strategy
- Using a left thoracoabdominal approach, tumor was removed and all lymph nodes in the specimen were negative microscopically for tumor.
- Patient had an uneventful recovery from the esophagogastrectomy in November 1987.
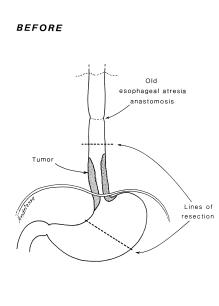
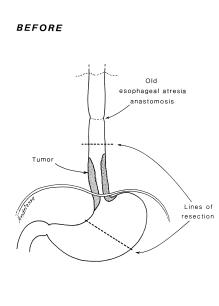
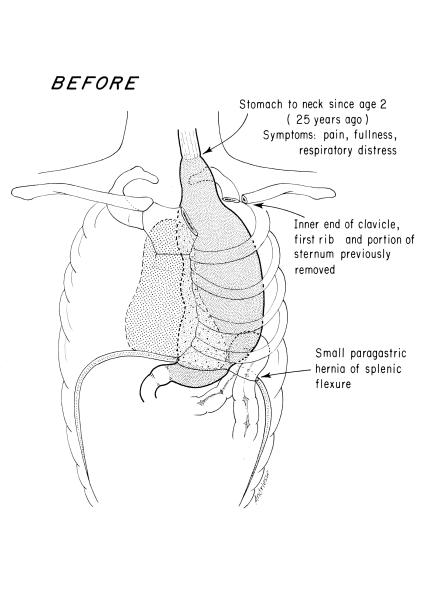
Fig. 3. Pre-Operative Anatomy (Select Image for High-quality Version). Diagram shows the extent of tumor and of resection to be performed using a thoracoabdominal exposure.
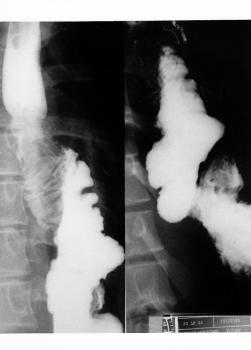
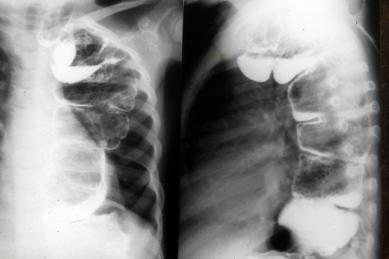
Fig. 4. Post-Operative Barium Swallow (Select Image for High-quality Version). This shows colon interposition from mid esophagus to remaining stomach.
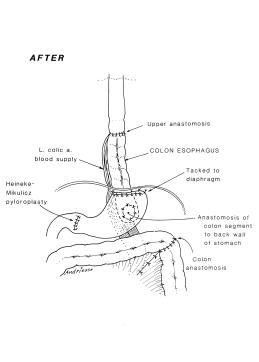
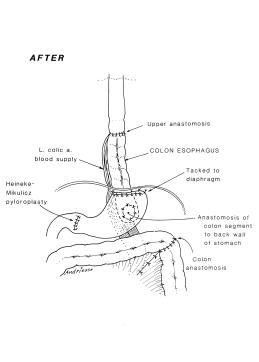
Fig. 5. Post-Operative Anatomy (Select Image for High-quality Version). Anatomy after tumor resection, and restoring gastrointestinal continuity with segment of transverse colon on left gastric pedicle. Note pyloroplasty to enhance gastric emptying.
Follow Up
- In 1992, 15 years later at age 26 years we performed a left thyroid gland total removal.
- Histology showed benign modular goiter.
- Patient last seen in 1994 and she was well.